In 2018, the Nobel Prize in physiology or medicine was awarded to two scientists for their pioneering work in the field of cancer immunotherapy for their contributions to the development of this revolutionary cancer treatment.
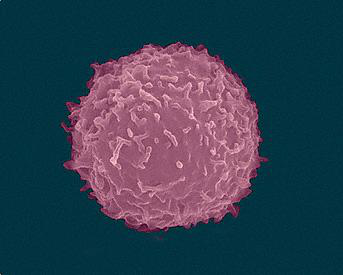
The mechanism of cancer immunotherapy is well understood. In the body's immune system, t-lymphocytes can attack cancer cells. But T cells have inhibitory receptors that inhibit T cell activity. Cancer cells are acutely aware of this, secreting substances that bind to these receptors and bind T cells. Immunotherapy, on the other hand, unlocks these bonds, allowing T cells to resume their ability to attack cancer cells.
As a revolutionary anti-cancer treatment, immunotherapy has two properties: on the one hand, the immune system has a "memory" for cancer. Once it works, it works for the long term. Some patients who received treatment did not relapse for nearly a decade, which is clinically equivalent to "cure". On the other hand, immunotherapy is not a panacea. According to statistics, only about 10% of patients can get long-term benefits from immunotherapy. So scientists and drug developers are developing new immunotherapies to benefit patients. Unfortunately, new drugs are not easy to develop. Several promising new drugs have failed in clinical trials. But that has not stopped innovation. A new combination of immunotherapies has emerged. The key behind this treatment is a receptor molecule called NKG2A, which is expressed in large amounts on the surface of T cells and NK cells, and the binding of NKG2A to ligands inhibits the function of T cells and NK cells. This is similar to the immune cell "brake" we mentioned above. Similarly, if NKG2A binding to ligand can be inhibited, it is expected to release the activity of immune cells. The researchers did an in vitro experiment first. They found that both NKG2A antibody and pd-l1 antibody alone increased the activity of immune cells. And both use together, can have apparent more outstanding effect. The researchers then tested it in a mouse model. This time, the NKG2A antibody alone had no effect, and the mice survived just as well as the control group.Pd-l1 alone saved about 30 percent of the mice's lives.
When the NKG2A antibody is combined with the pd-l1 antibody, That number jumps from 30% to 70%. This result also indicates that NKG2A antibody is expected to synergize with classical tumor immunotherapy.
With these positive results, the scientists decided to apply this strategy to the treatment of human cancer patients. In vitro experiments, this antibody showed the expected effect, effectively enhancing the anti-tumor ability of T cells and natural killer cells. Safety and efficacy were assessed in early clinical trials.
Scientists have observed promising progress. Six of the 20 patients had partial remission, more than 30 percent. Fifteen patients had stable disease control, more than 60 percent.
The researchers conclude that NKG2A is an immunocheckpoint inhibitor that promotes the anti-tumor activity of T cells and natural killer cells. This is expected to complement existing immunotherapy to better treat cancer patients.







